Uterine fibroids, medically termed leiomyoma, fibromyoma or myoma but commonly known as fibroids, are benign (non-cancerous) tumours that grow within the muscular layer of the uterus. Fibroids are composed of muscle and fibrous tissue, which give them a firm texture.
Fibroids are the most common of benign tumours found in women. They usually occur during the middle or late reproductive years of a woman (over the age of 30), although some young women in their 20s also develop fibroids. These tumours usually come in multiples (can be up to a hundred), and can vary hugely in size: from tiny pea-sized to larger than a melon.
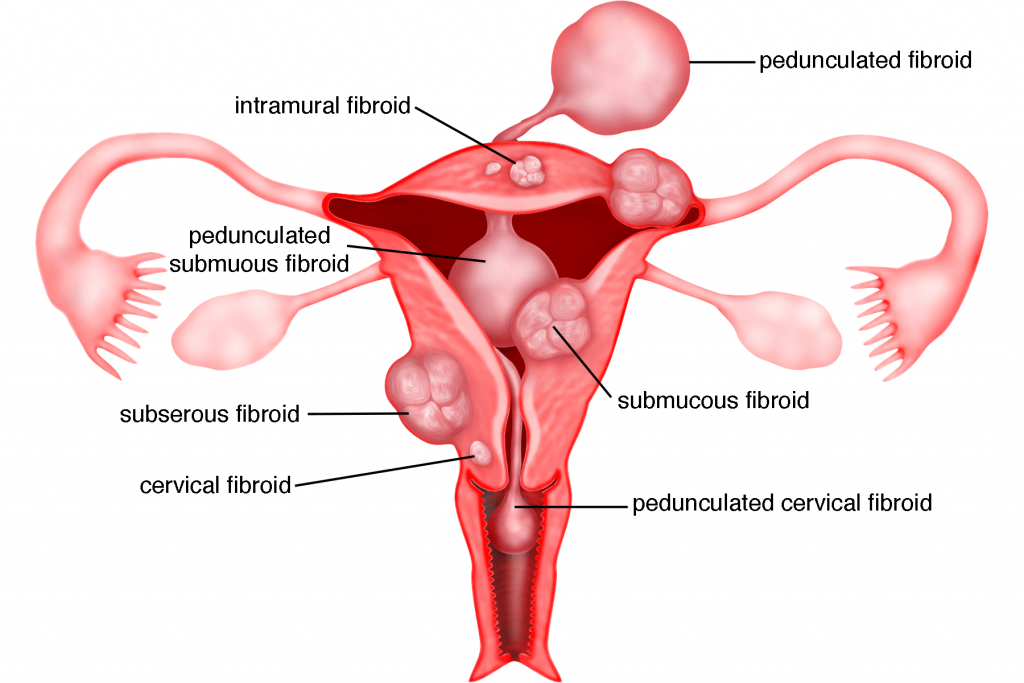
Types of Fibroids
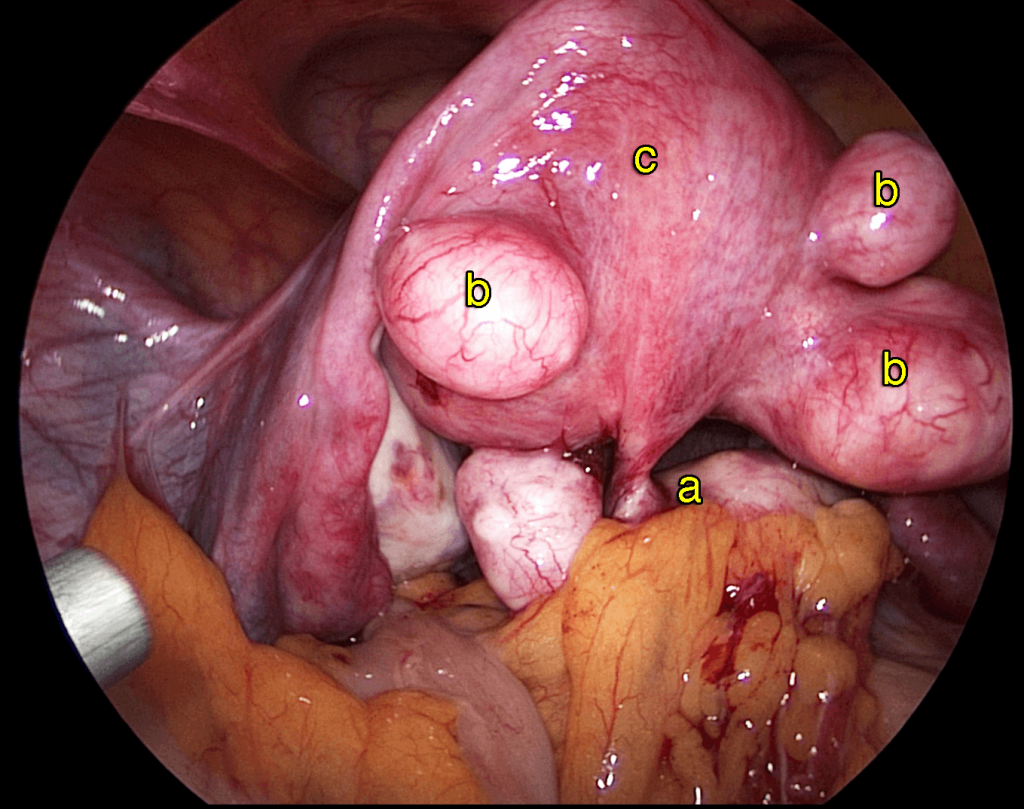
Fibroids are classified according to the location where they grow within the uterus. There are three main types of fibroids:
1) Submucous fibroids
Fibroids that grow towards or just beneath the lining of the uterus (endometrium).
2) Intramural fibroids
Fibroids that grow deep within the muscular wall of the uterus.
3) Subserous fibroids
Fibroids that grow towards or just beneath the outer layer of the uterus (perimetrium).
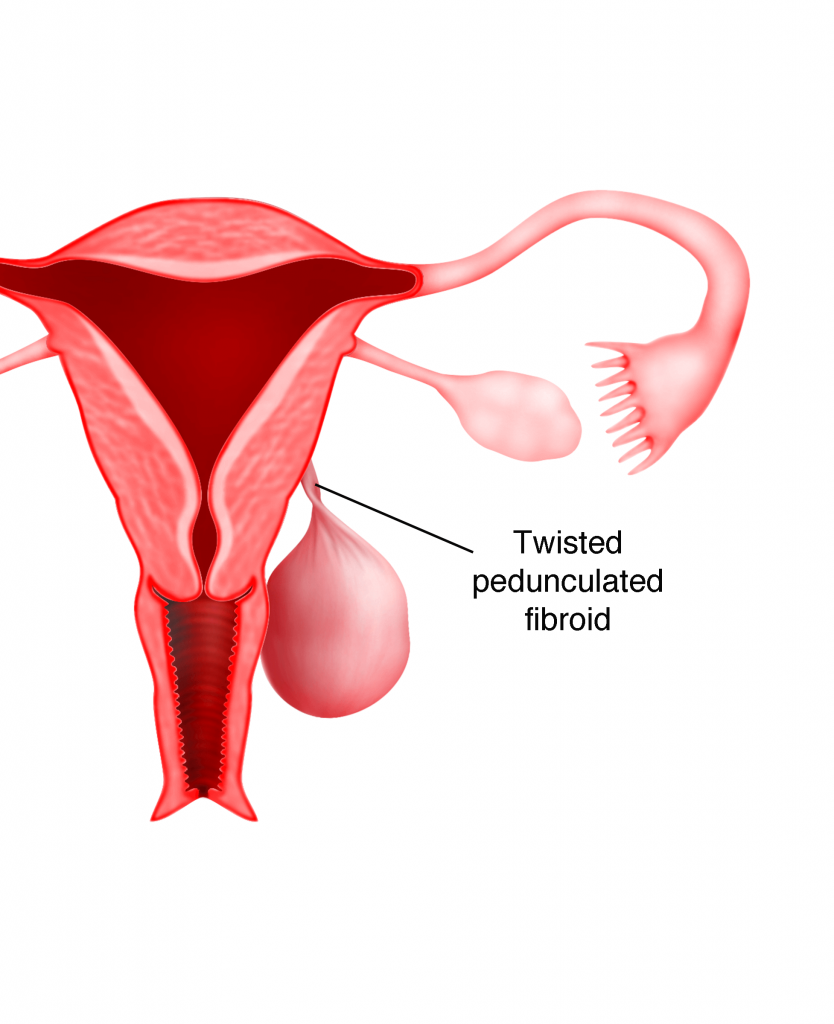
Some fibroids are attached to the uterus by a thin stalk called the peduncle. These fibroids are generally known as pedunculated fibroids.
Fibroids that grow within the cervix (which are relatively rare) are known as cervical fibroids.
The actual cause of fibroids cannot be completely determined. Factors such as heredity, race, and oestrogen level, however, are conclusively linked to the disease.
1) Heredity
It has been found that many women with fibroids have a family history of the disease. It is believed that fibroid arises from the mutation of a single muscle cell, which exists from birth.
2) Race
Researchers have suggested that women with African-American ethnicity are 2-3 times more likely than other women to develop uterine fibroids. Although the actual reason behind the heightened likelihood is unknown, it has been speculated that the genetic predisposition could play a role in it, since it is common for African-American women to develop fibroids at a younger age. These women also tend to have multiple and large-sized fibroids.
3) Oestrogen Level
Many women who develop fibroids are also found to have elevated oestrogen levels. While it is unclear how oestrogen contributes to the origin of the disease, it has been confirmed that fibroids do depend on the hormone to grow, just like endometriosis. This also explains why some women experience worse symptoms of fibroid during perimenopause (menopause transition years), as their oestrogen levels are abnormally high at this stage. The symptoms, however, settle down naturally after menopause due to a significant decline in oestrogen levels. Under oestrogen deficiency, fibroids usually shrink, and sometimes disappear without treatment.
Case 2.1 : 5 of 6 sisters with fibroids
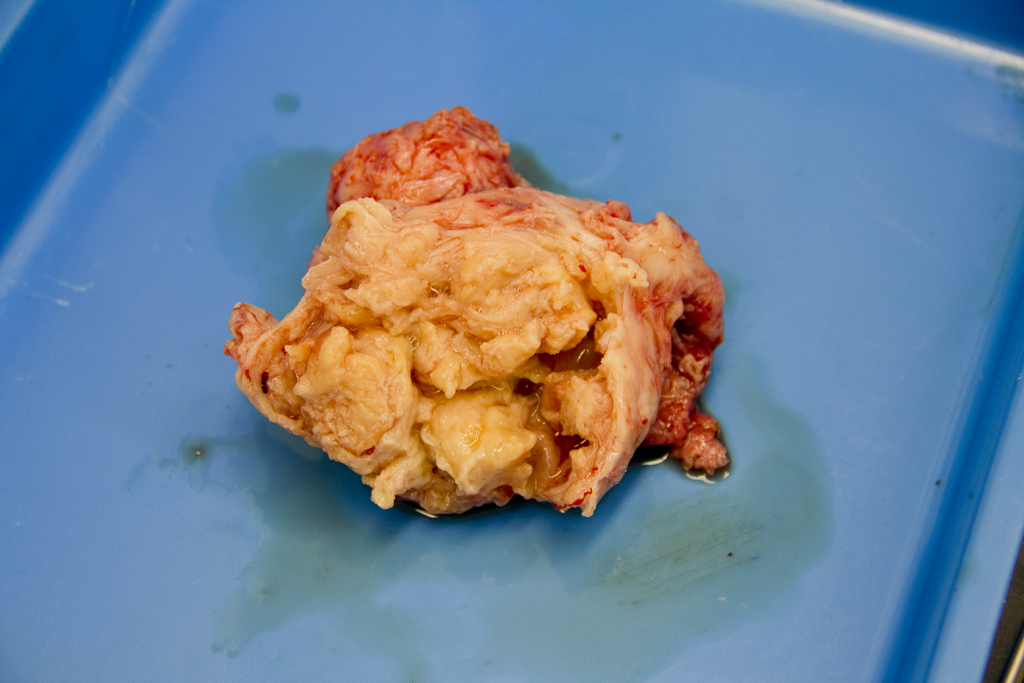
Miss LSP was a 46 year old single lady who came to see me in June 2003 with a problem of abdominal distension. Her menses was regular but heavy with occasional clots. Examination revealed a pelvic mass that reached up to 4 cm above the umbilicus (g), (24 gestational weeks size – like a 6 month pregnancy). Abdominal ultrasound showed an enlarged uterus with multiple huge fibroids. She underwent a laparotomy and myomectomy. 24 fibroids of varying sizes the largest 13 cm in
longest diameter were removed (see Figure: 2.9). Postoperatively, she was well. She is on regular follow up. Her fibroids have recurred since 2005. However, the largest has remained the same size (4.5 x 4.6cm) for many years. She attained menopause in 2008 at the age of 51.
Miss LSL saw me in 2003 after her sister was diagnosed with fibroids. She was 37 years old and single. Her periods were regular and not heavy. Examination revealed a large pelvic mass reaching 2 cm above the umbilicus (22 gestational weeks size). Ultrasound showed multiple uterine fibroids. She also underwent a myomectomy. 20 fibroids were removed and the total weight of the fibroids was 3.9kg (see Figure 24.8). The largest measured 25 cm in the longest diameter. Postoperatively she was well and was on regular follow up. The fibroids recurred. In 2010, there were again numerous fibroids and the uterus reached 4 cm below the umbilicus (16 gestational weeks size). She was 44 years old at that time and was still single. She was advised a hysterectomy but decided to do another myomectomy. 40 fibroids were removed size ranging from 15 mm to 8 cm in diameter with a total weight of 1.01 kg. Postoperatively she has been well and on regular follow up.
Miss LTH first saw me in 2004 at the age of 45 years. She could not pass urine for a few days. Examination and ultrasound showed multiple uterine fibroids with a large cervical fibroid measuring 9cm in diameter. She underwent a total abdominal hysterectomy.
LTB was 44 years old in 2006 when she saw me for a routine gynaecological examination. She was married with no children. Ultrasound showed multiple small uterine fibroids the largest measuring 1.57 cm. in diameter. She was asymptomatic and the fibroids remain small till today.
LSF has 2 children and she saw me in 2007 at 38 years of age for a routine gynaecological examination. Examination and ultrasound showed 2 small fibroids the largest measuring 2.69 cm. She was seen again in 2013 at the age of 44. She was asymptomatic but her fibroids have increased in number and size, the largest being 3.26 x 3.79 cm. She was seen again in December 2014. Her fibroids had increased in size and the largest was 3.85 x 5.63 cm. However, she was asymptomatic and is on follow up.
Signs and Symptoms
Many women with fibroids do not experience unusual signs or symptoms and mostly only discover the existence of the fibroids incidentally, during a routine pelvic or ultrasound examination. However, the appearance of symptoms is certainly possible and can sometimes be highly troubling. The most common symptoms of fibroids are as follows:
1) Heavy and prolonged menstrual bleeding
Women with fibroids are likely to experience abnormally heavy and prolonged menstrual bleeding (7 or more days), which can lead to iron-deficiency anaemia. This symptom is widely believed to be caused by the inability of the muscles of the uterus to contract effectively to reduce menstrual flow, due to the presence of fibroids within the muscular wall of the uterus.
2) Pelvic pressure
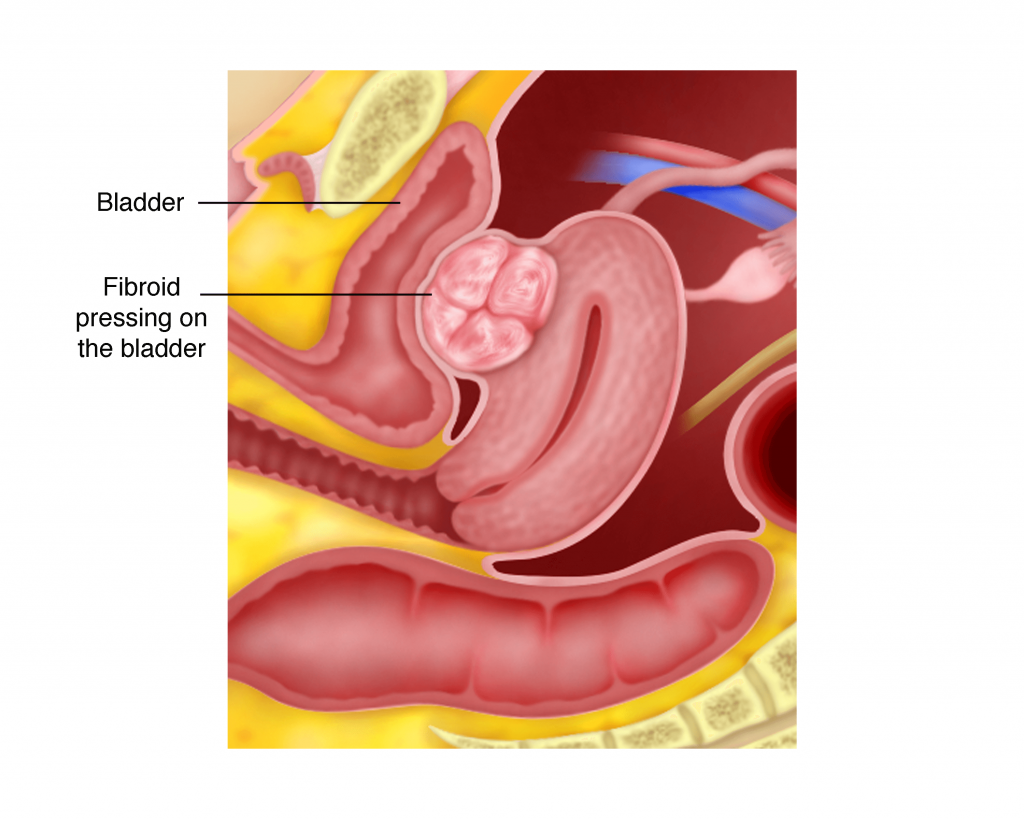
Women with large fibroids may feel a sense of fullness or pressure in the pelvic area, as the fibroids press against the surrounding organs, such as the bladder and rectum. This pressure may even damage the organs. Symptoms of this kind of pressure are:
a) Difficulty in urinating
When the fibroid presses on the bladder, the bladder capacity is reduced. Consequently, the subject may have the urge to urinate more frequently or feel incomplete bladder emptying. In rare cases where the urethra (g) is blocked, the subject will experience acute urinary retention (sudden inability to urinate).
Case 2.2 : Fibroids that cause sudden inability to urinate
MS, a 43 year old lady, married with no children, came to seevme in August 2014 with a problem of several episodes of inability to pass urine requiring catheterization. She also complained of needing to go to the toilet up to 12 times a day. Examination revealed a large 14 x 8 cm posterior cervical fibroid and another fundal fibroid measuring 8 x 6 cm. She could not decide whether to undergo a myomectomy or a hysterectomy. She finally decided to undergo a hysterectomy. A total laparoscopic hysterectomy (g) was performed in October 2014. Postoperatively, she still could not pass urine. She was sent home with a catheter. The catheter was later removed and even though she could pass urine after removal of the catheter, she could only pass in small amounts. She was taught self-catheterization. Every time after she passed urine, she had to catheterize by herself and to measure the amount of urine that came out (residual urine). Her residual urine became lesser with time.
Discussion
Fibroids can press on the bladder and can cause frequent urge to pass urine. It can sometimes cause retention of urine. Chronic retention of urine as a result of fibroids can cause difficulty in passing urine even after the fibroid is removed. Patients who develop sudden retention of urine because of a fibroid should remove the fibroid or the uterus as soon as possible.
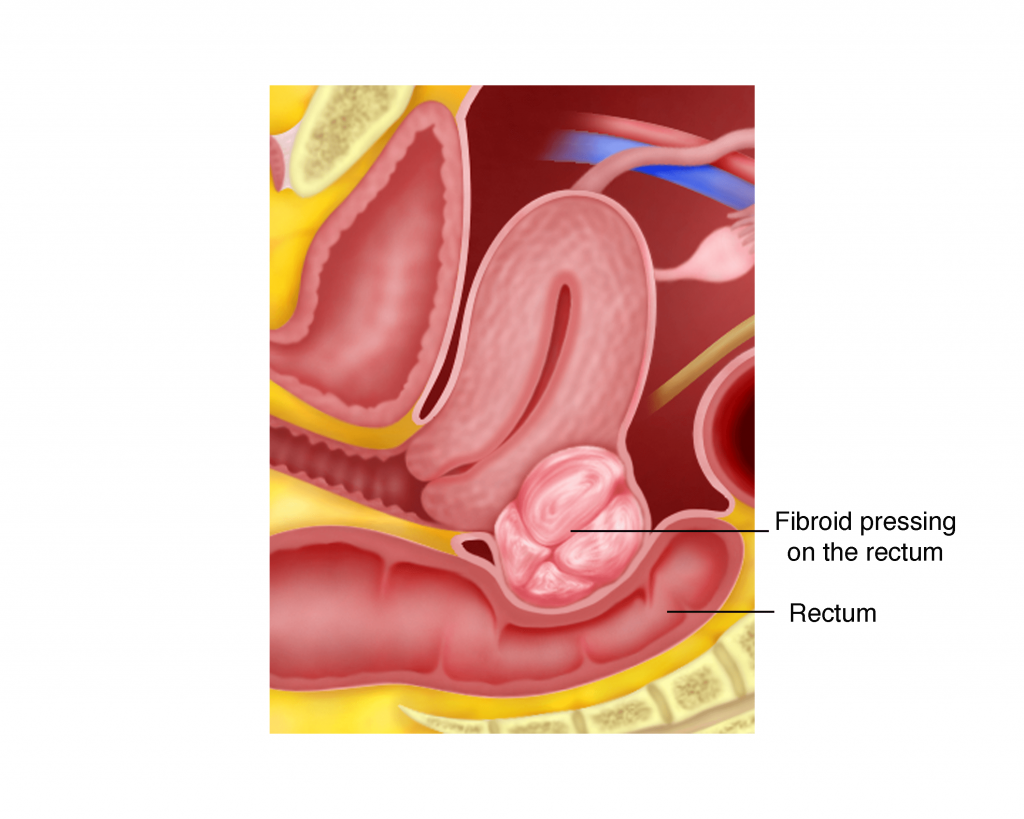
b) Constipation due to pressure on the rectum.
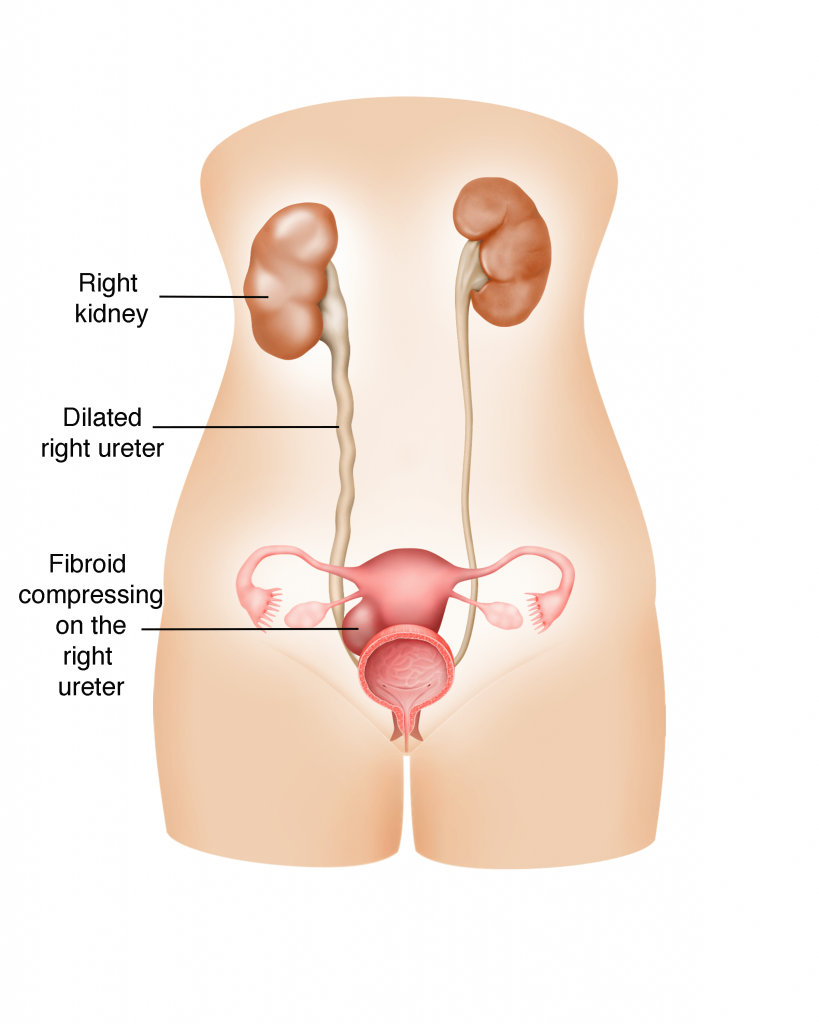
c) Dilation of the kidney with urine (hydronephrosis)
Occasionally, the fibroid presses on the ureter and obstructs the passage of urine from the kidney to the bladder. Urine will start accumulating behind the obstruction and eventually distend the entire kidney. This is known as hydronephrosis and can result in urinary tract infection and/or even cause permanent damage to the kidney.
3) Pelvic pain
There are a few reasons why fibroids cause pain in the pelvic area.
a) Fibroid degeneration
When a fibroid grows to a size that its blood supply is no longer sufficient and blood can no longer reach the fibroid’s central area, it will start to degenerate from inside. In other words, the muscle tissue that makes up the fibroid dies due to lack of oxygen. The process will cause severe pain that usually lasts between several days to a week or even more.
b) Twisted peduncle
When a pedunculated fibroid becomes twisted, it can cause excruciating pain to the sufferer that an immediate surgery to remove the fibroid is required. Another situation that can occur is when the twisted peduncle blocks the essential blood supply to the fibroid causing fibroid degeneration, which in itself, is very painful.
c) Fibroid infection
Occasionally, a degenerating or dying fibroid can infect the surrounding uterine tissue, causing pain.
d) Malignant change in fibroid
Very rarely does a fibroid evolve into a malignant (cancerous) tumour called leiomyosarcoma. There is a one –in –a thousand chance of this occurring. When this does happen however and the malignant tissue starts to invade the surrounding uterine tissue, it can result in intense pelvic and abdominal pain, which may be accompanied by abnormal vaginal bleeding.
Can the diagnosis of a uterine sarcoma (cancer of the fibroid) be made without surgery?
Fibroids are very common and are mostly benign. They are usually suspected during an abdominal and a pelvic examination and confirmed on an ultrasound examination. There is no conclusive test that can be done to confirm if a fibroid is a cancer (sarcoma). In postmenopausal women where fibroids are growing, a cancer can be suspected but it still cannot be confirmed until surgery is done to remove the fibroid or the uterus. There are ongoing studies to diagnose a uterine sarcoma before surgery. One such study looked at performing MRI using a dye called Gadolinium and a LDH blood test to predict whether a fibroid is a sarcoma. However, this test is still not commonly available.
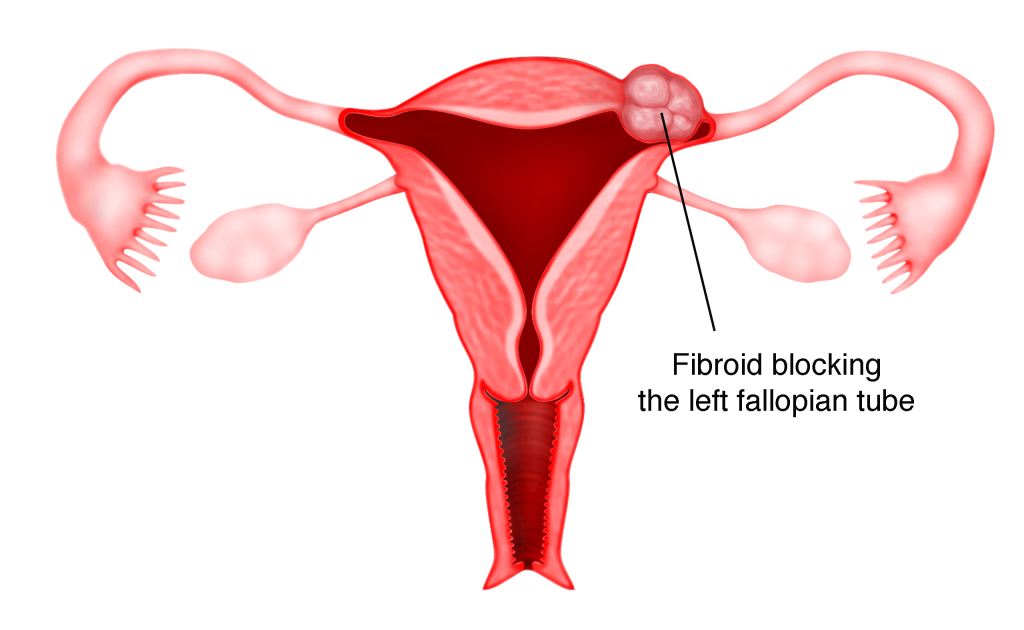
4) Infertility
Fibroids growing in the Fallopian tubes can compress and block the passage of the egg and sperms, making fertilization impossible. Fibroids growing within the muscular wall of the uterus may also severely distort the uterine cavity, especially the endometrium (the lining of uterus) and interfere with the blood supply to it, making implantation difficult or impossible.
Diagnosis
1) Family Medical History
Since fibroids tend to run in families, a patient’s family medical history is significant in helping a gynaecologist determine the likelihood of fibroids.
2) Pelvic Examination
Fibroids of asymptomatic patients are usually discovered during their routine pelvic examinations, when their gynaecologists find round and lumpy masses in their lower abdomen. However, the presence of fibroids cannot be confirmed via pelvic examination alone as other diseases, such as adenomyosis or ovarian cysts (if lumps are felt on the sides of the lower abdomen) can be mistaken for fibroids or the other way round. Other assessment techniques such as reviewing a patient’s family medical history, ultrasound scanning and magnetic resonance imaging (MRI) are required to corroborate the diagnosis.
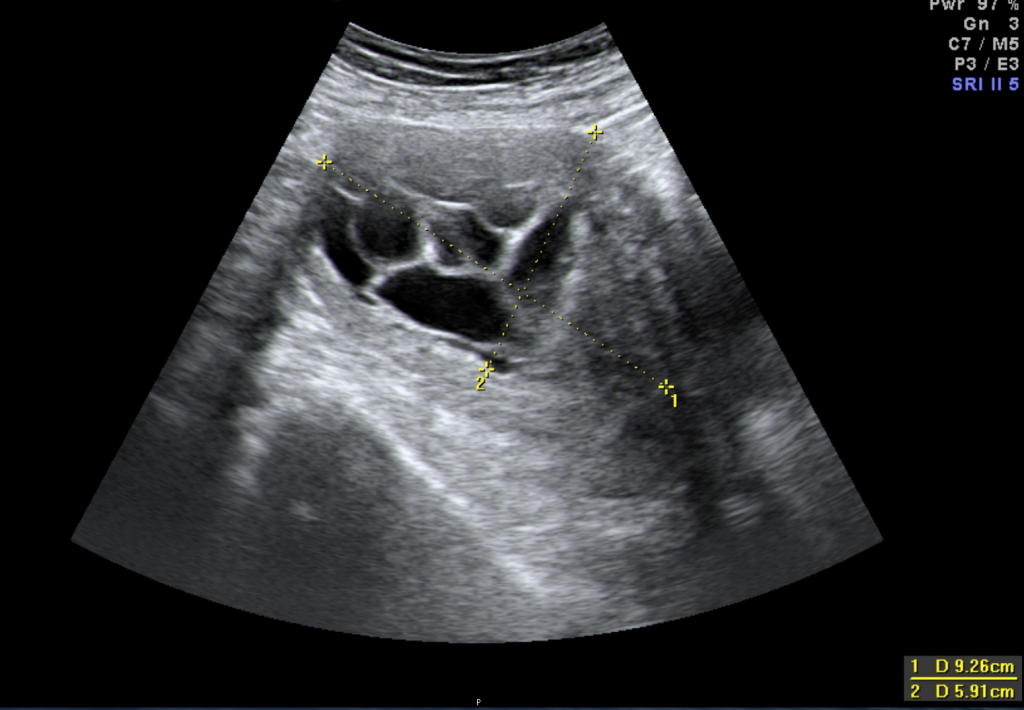
3) Ultrasound scanning
Most fibroids are easily detectable with ultrasound. The scanning can be performed either abdominally or transvaginally (through the vagina). A transvaginal ultrasound can provide greater clarity of the size and location of each fibroid because the probe is closer to the uterus. The ultrasound results combined with the findings from the pelvic examination are usually sufficient to diagnose fibroids.
4) Magnetic Resonance Imaging (MRI)
Sometimes MRI may be required for definite confirmation. MRI is so far, the most accurate diagnostic tool for fibroids. It provides far more detailed images of fibroids than the ultrasound, enabling a gynaecologist to determine the exact number of fibroids, their size and position as well as the degree of anatomical distortion of the uterus and its surrounding organs caused by these fibroids.
5) Hysteroscopy
Hysteroscopy is a technique that allows a gynaecologist to directly view a patient’s uterine cavity by inserting a narrow tube-like telescopic camera (hysteroscope) into the uterus through the cervix. It is very useful for assessing submucous fibroids (Figure 41.5) and the overlying endometrium. This technique is usually necessary for patients who claim to have abnormal vaginal bleeding and/or recurrent miscarriage (see page 417).
Treatment Options
Surgery is considered the standard treatment for women suffering from fibroids. Two most common procedures to surgically remove fibroids are hysterectomy and myomectomy. Transcervical resection of the fibroid can be performed in small submucous fibroids. An alternative to surgery is uterine artery embolization (UAE).
1) Hysterectomy
Hysterectomy is the procedure of removing the entire uterus including the cervix. This can be performed either with the help of a laparoscope (see chapter 33) or by laparotomy. Hysterectomy is usually an option for women who have completed their family and are above 40 years of age. The advantage of hysterectomy over myomectomy is that it eliminates the possibility of fibroid recurrence and puts an end to all symptoms including heavy menstrual bleeding, which may persist even after a myomectomy is done.
2) Myomectomy
Myomectomy is the procedure of removing the fibroids without removing the uterus. It can be performed either laparoscopically (see chapter 24) or by laparotomy. The main advantage of myomectomy is that it allows a patient to conceive in future. One disadvantage of the procedure is that, it may cause considerable blood loss during surgery that blood transfusion may be necessary. Other disadvantages are the possible recurrence of fibroids and the possible persistence of heavy menstrual bleeding after surgery. In cases of recurrence, subsequent myomectomy will be more complicated as the previous one may have led to the formation of adhesions (scar tissue) (g).

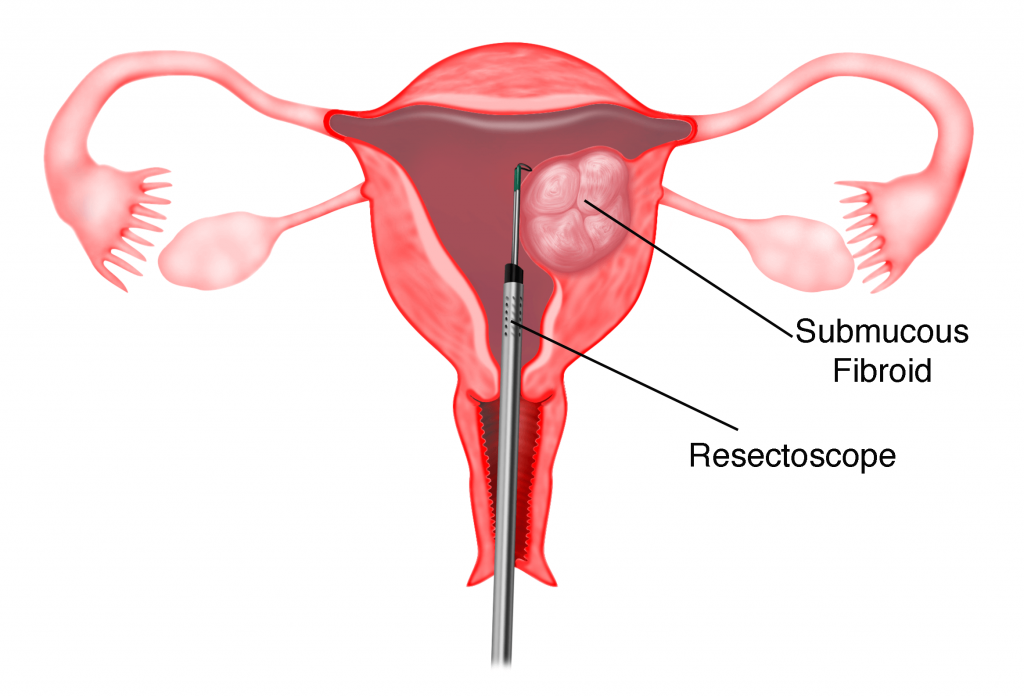
3) Transcervical resection of fibroid
In submucous fibroids, hysteroscopic resection of the fibroids can be performed (see chapter 41). This is usually done when the submucous fibroids are small. An instrument called a resectoscope is used to cut the fibroid into small pieces until the base of the fibroid is reached. The small chips of the fibroids are then removed through the vagina.

4) Uterine Artery Embolization (UAE)
UAE is conducted under a moving X-ray (fluoroscopy) by an experienced interventional radiologist. It is a procedure where a tiny tube called catheter is inserted through an incision in the groin area into the femoral artery and then threaded to the uterine arteries. Some tiny sand-like gelatinous particles will be injected into the uterine arteries through the catheter in order to block the blood supply to the fibroids.
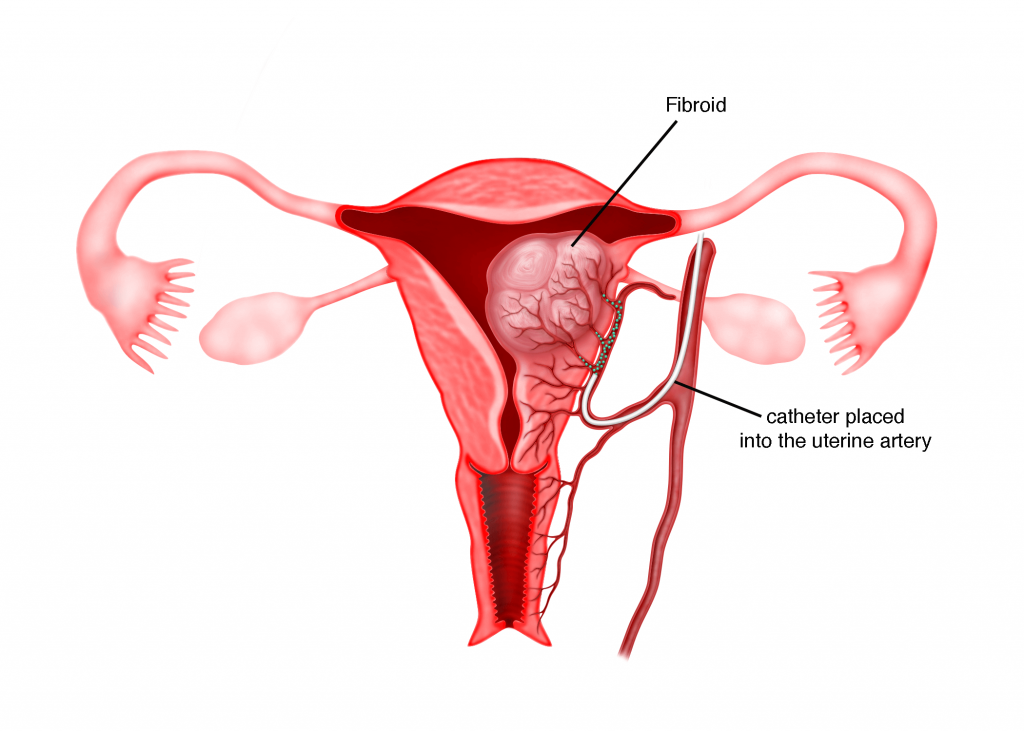
The blockage or embolization will eventually result in the degeneration of the fibroids. The advantages of UAE are minimal blood loss, fertility is not affected and the recovery period is
short. The disadvantages are that patient may experience post- embolization syndrome (PES) such as severe pelvic pain and cramping, as well as nausea and vomiting that lasts for several days following the procedure. Embolization may cause damage to the uterus and uterine infection may also occur. When the fibroids begin to degenerate, they can cause severe pain to the patient.
As fibroids normally will lyse by themselves (self-destruct) after menopause, surgery is usually not recommended for small (less than 5 cm) and asymptomatic fibroids. For these fibroids, no treatment except constant surveillance of their growth is required.
Summary
Fibroids are common benign tumours in women. They are usually asymptomatic and do not require treatment. When they become symptomatic, surgery may be necessary
