What is Hysteroscopy?
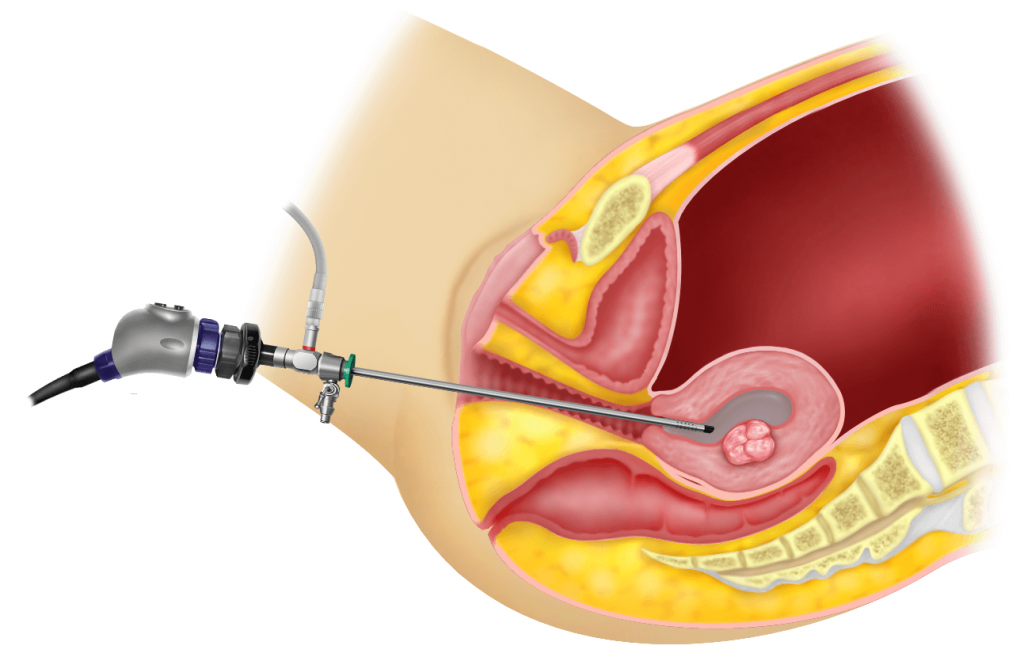
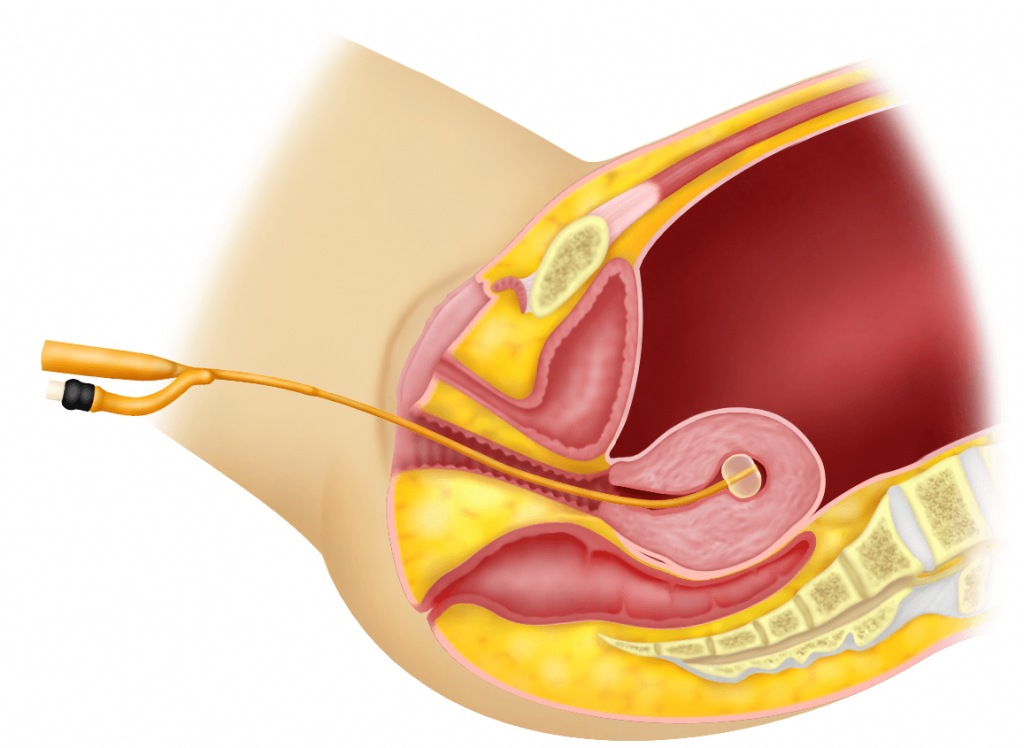
Hysteroscopy is a procedure whereby a narrow telescope (called a hysteroscope) attached to a camera is passed via the cervix into the uterus to visualize the inside of the uterus (endometrial cavity).
Types of hysteroscopy
There are two reasons why hysteroscopy is performed.
1) Diagnostic hysteroscopy – to make a diagnosis of a symptom.
2) Operative hysteroscopy – to perform a surgery.
Indications for performing hysteroscopy
The reason for performing hysteroscopy will depend on whether it is for diagnosis or surgery. This is discussed in chapter 37 (diagnostic hysteroscopy) and chapter 38 (operative hysteroscopy).
The best time to perform a hysteroscopy
1) Just after menses (before ovulation) – the endometrium is thinnest just after menses and so the cavity can be seen well. This also removes the worry of performing a hysteroscopy during a pregnancy.
2) In post menopausal women, hysteroscopy can be performed at anytime
3) In patients who have irregular or prolonged bleeding, hormones should be given to stop the bleeding before hysteroscopy is performed. However, if bleeding persists, hysteroscopy should be performed despite the bleeding.
When is hysteroscopy not advisable?
1) During menses or per vaginal bleeding – It will be difficult to visualise the endometrial cavity during menses.
2) Pregnancy – If pregnancy is suspected hysteroscopy must be avoided because the procedure may injure the foetus.
3) Pelvic Inflammatory Disease (PID) – In patients who have PID or are suspected to have PID, hysteroscopy must be avoided to prevent the infection from flaring up.
4) Cancer of the cervix – In patients suspected of having cancer of the cervix hysteroscopy should not be done.
5) Acute herpes infection
6) Heavy vaginal discharge – this may be caused by sexually transmitted disease (eg trichomonas, gonorrhoea, chlamydia). A swab must be taken for culture and treatment must be given before the hysteroscopy.
Complications
Complications can occur during both diagnostic and operative hysteroscopy. Complications can be divided into :
1) intraoperative (occurring during the procedure)
2) postoperative (occurring after the procedure)
1) Intra-operative Complications
a) Pain
Diagnostic hysteroscopy is usually performed without anaesthesia. The internal Os (g) may be narrow and some pain or discomfort may be felt when the surgeon passes the hysteroscope through the internal Os (see Chapter 1). Some factors that may increase the chances of pain during office hysteroscopy include, nulliparity (patient has never delivered a baby), menopause, history of pelvic inflammatory disease and anxiety.
b) Vasovagal crisis
This is a sudden feeling of lightheadedness, nausea and fainting and this is related to pain that may occur when the hysteroscope is passed into the uterine cavity.
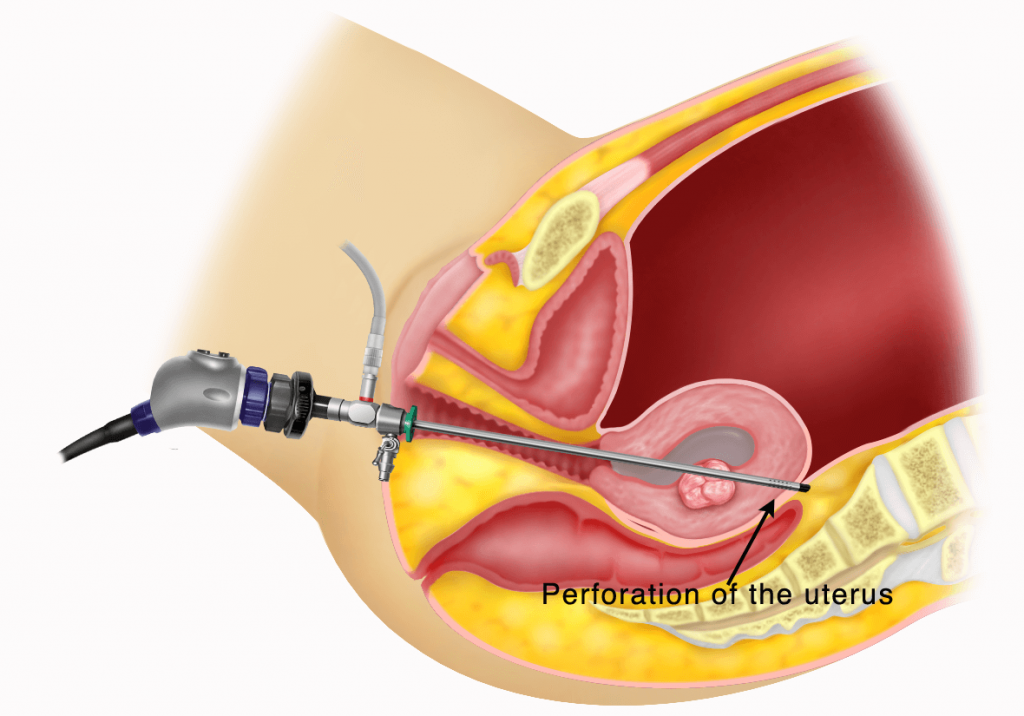
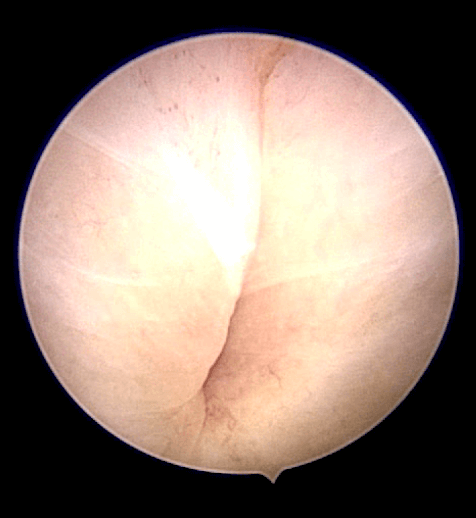
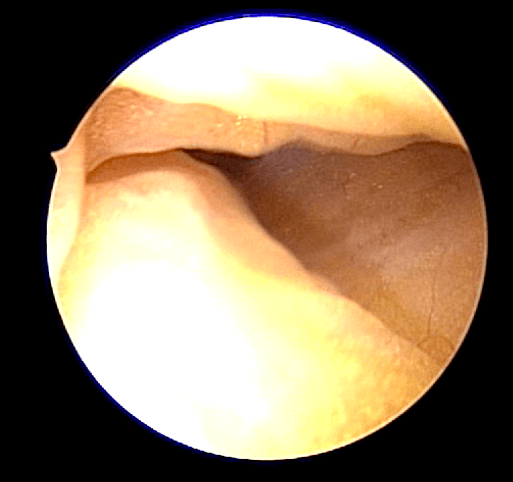
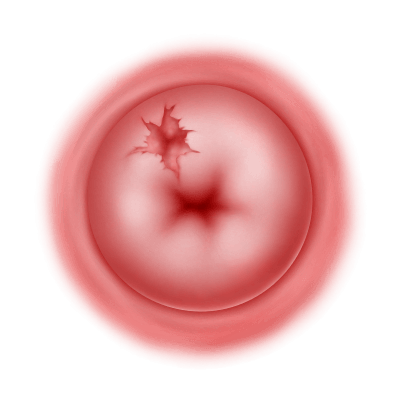
c) Perforation of the uterus
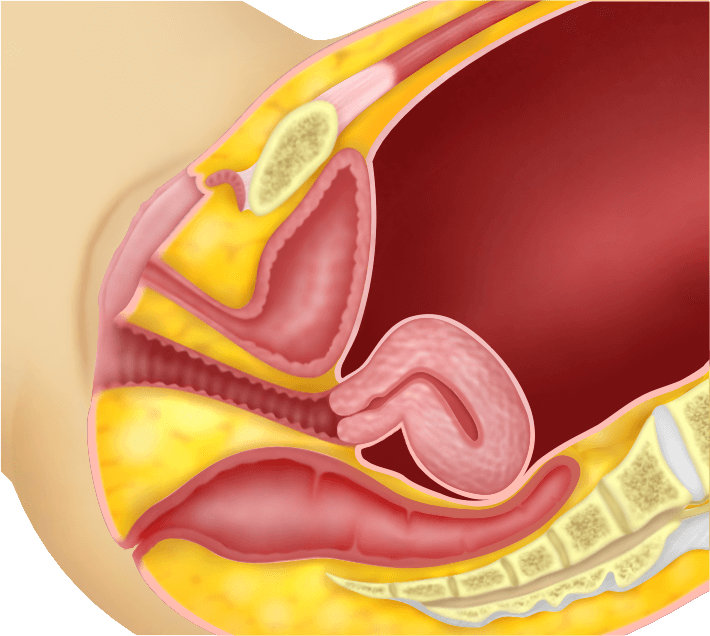
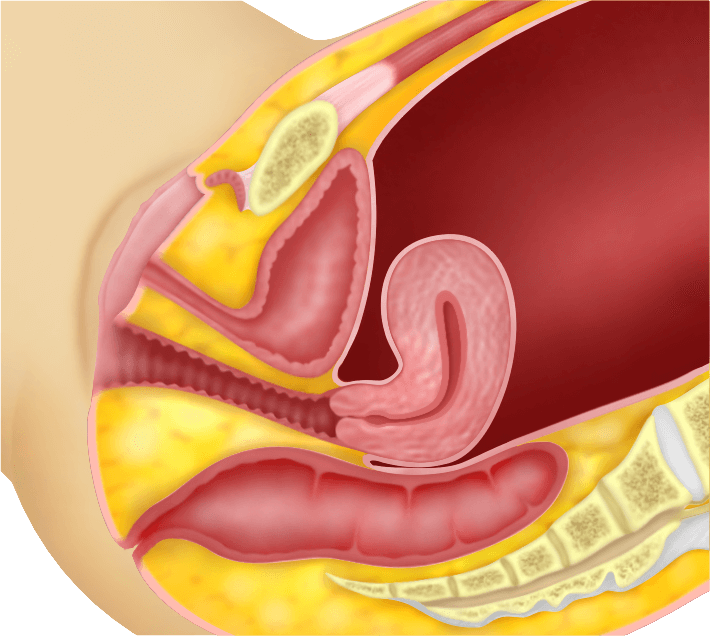
Perforation of the uterus may occur while performing hysteroscopy. This usually occurs when the cervical Os (see Chapter 1) is very tight and manipulation can cause perforation. Sometimes it may be due to the abnormal position of the uterus. When the uterus is acutely bent backwards (retroverted and retroflexed (Figure. 36.3)) or acutely bent forward (anteverted and anteflexed) (Figure. 36.4), a perforation may occur. When perforation occurs during a diagnostic hysteroscopy (Figure 36.5, 36.6 and 36.7), the procedure must be stopped and no further action is necessary. The patient will be asked to rest and be observed for a few hours to ensure that there is no internal bleeding. A perforation may also occur during
an operative procedure (eg transcervical resection of a fibroid (see chapter 41) or excision of a uterine septum (see chapter 40) If this occurs, a laparoscopy may be necessary to ensure that the perforation has not injured any internal organ (eg bowel or blood vessels) and there is no internal bleeding. The perforation can be sutured laparoscopically.
d) Trauma to the cervix
A large hysteroscope is used during an operative hysteroscopy. Dilatation of the external and internal Os is necessary to pass the operative hysteroscope. The cervix is usually held with an instrument (eg tenaculum) when the internal Os is dilated. The cervix may be torn at this time. Such tears are usually sutured vaginally.
e) Haemorrhage
During operative hysteroscopy (eg transcervical resection of a fibroid) bleeding may occur. This bleeding can sometimes be heavy. Such bleeding can be stopped by placing a catheter into the uterine cavity and distending it with saline so as to apply pressure to the endometrial cavity. The catheter is usually placed from 6 hours to 24 hours. Bleeding will usually stop and the catheter can be removed. However if bleeding persists, a hysterectomy may be necessary.
f) Fluid overload
During operative hysteroscopy, glycine or saline is used to distend the uterus. This fluid can be absorbed by blood vessels that may be opened during the surgery. Too much absorption of this fluid, leads to fluid overload and the patient can become ill. She may become confused and puffy. This condition may require admission to the intensive care unit for observation. This is a very dangerous complication. When this complication is suspected, the surgery is stopped immediately and measures are taken to remove the extra fluid that has entered the body of the patient.
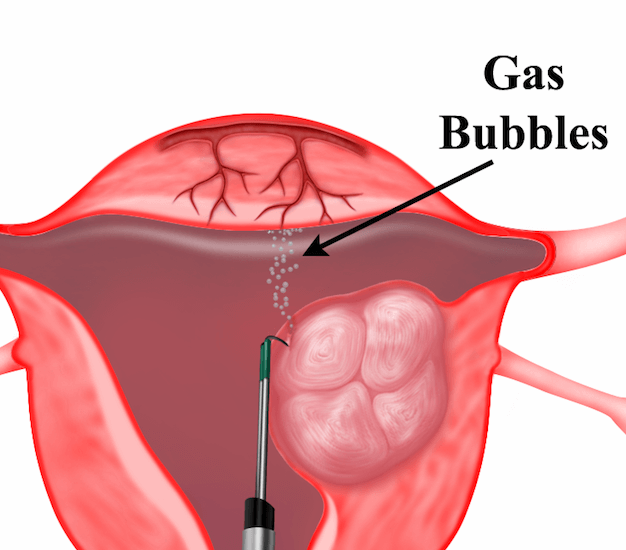
g) Gas embolism
This is a rare and very dangerous complication. Air may accidentally be drawn into the veins and this can go into the heart and lungs. This can be fatal.
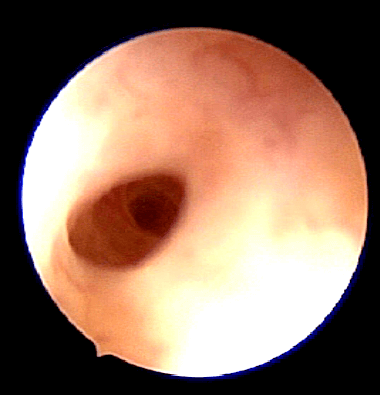
Case 36.1 Uterine perforation during office hysteroscopy
Madam ZF underwent a Diagnostic Hysteroscopy for the diagnostic evaluation of her infertility. The cervical Os was very tight and during manipulation to enter the cavity of the uterus a perforation of the uterine cavity was noted (Figure. 36.6 and Figure. 36.7). The hysteroscope was immediately removed. A transvaginal ultrasound was performed and fluid was seen in the Pouch of Douglas (g). The patient did not have much abdominal pain. She was rested for 2 hours and then re- evaluated. She did not have any abdominal pain and her vital signs were normal. She was allowed to go home and requested to return if she had any symptoms. She was seen again in a week and was well.
Discussion
In difficult cases especially when the uterus is acutely anteverted or retroverted, Diagnostic Hysteroscopy can be performed with the assistance of an abdominal ultrasound. If it is still difficult to enter the uterine cavity then the operation should be performed under general anaesthesia, while simultaneously a laparoscopy should be performed.
2) Post operative Complications
a) Haemorrhage
Patients who have been discharged can develop bleeding at home. This will require immediate admission and treatment.
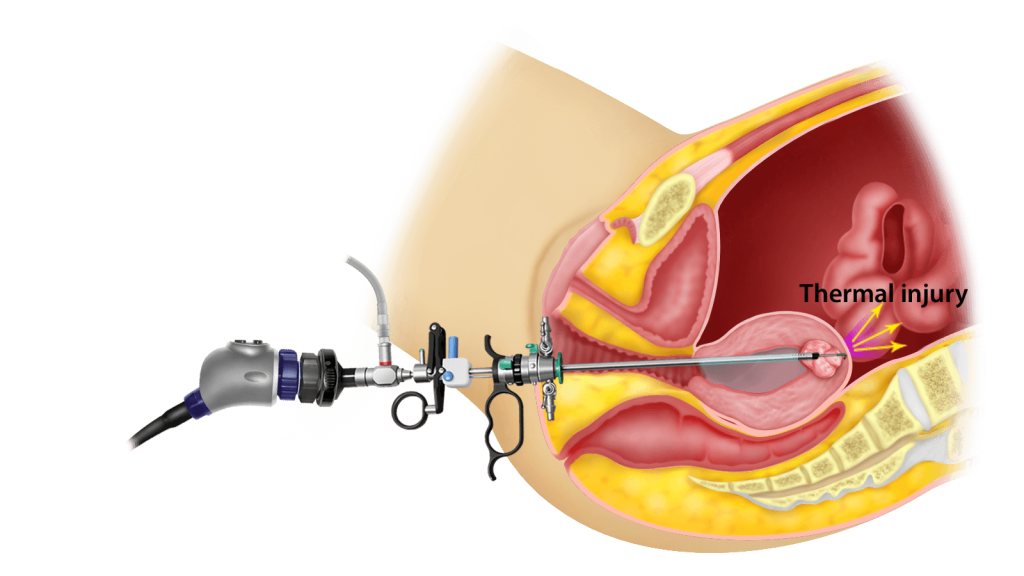
b) Thermal damage to the bowel
During operative hysteroscopy using electric current (eg transcervical resection of a fibroid) an unknown thermal injury to the bowel may occur and this may not be noticed during the surgery. After several days, the patient may suffer from abdominal pain and fever. This may require another surgery (laparoscopy or laparotomy).
c) Infection
Infection of the endometrial cavity rarely occurs after the surgery. This can present as fever and pelvic pain, and can usually be resolved with antibiotics.
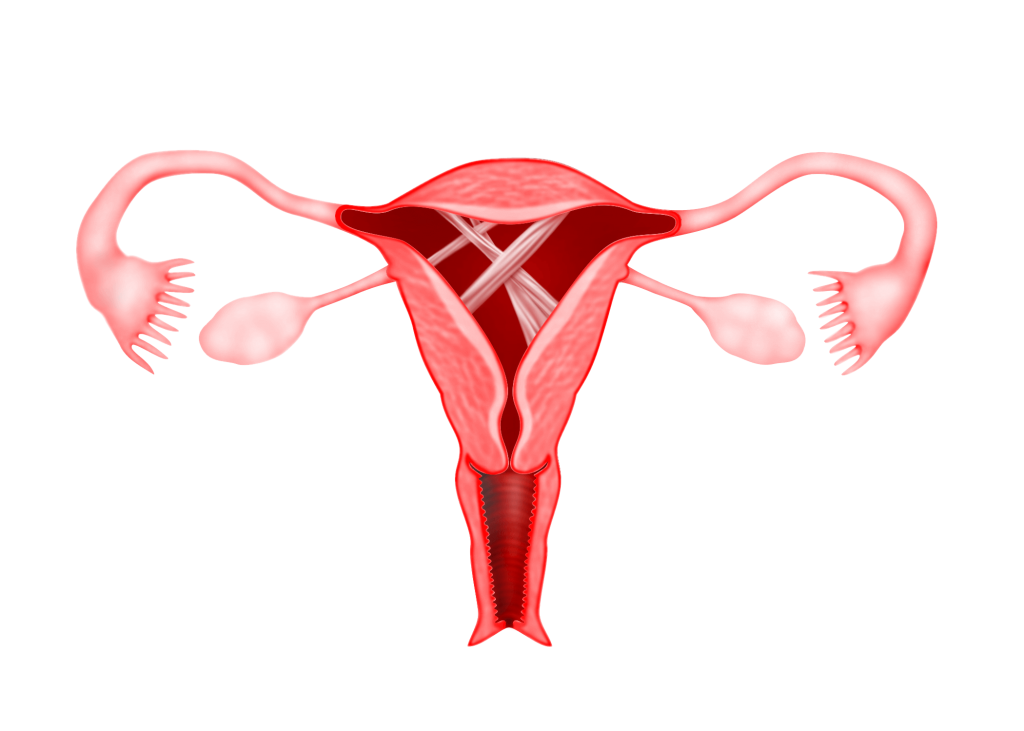
d) Intrauterine adhesions
After operative hysteroscopy, intrauterine adhesions can occur. This may lead to decrease in uterine bleeding and some times amenorrhoea (cessation of menses).
Post operative advise
Some women may experience cramping similar to period pain after the procedure. There may be shoulder pain, which is caused by the fluid, or gas that is used to inflate the uterus. This pain will subside in a few days.
There may be some bleeding after the hysteroscopy especially when hysteroscopic surgery is performed. Bleeding usually subsides in a few days.
Sexual intercourse must be avoided till bleeding and vaginal discharge stop.
In patients who have a higher risk of pelvic infection (eg tubal block or hydrosalpinx) antibiotics may be given before and after the procedure.
Tampons should be avoided for at least a month after the hysteroscopy, to help reduce the risk of infection.
Severe lower abdominal pain, pain during urination, fever, vaginal discharge that is smelly or unpleasant and heavy bleeding are symptoms that will require the immediate attention of a doctor.

Summary
Hysteroscopy is a technique whereby a fine telescope attached to a camera is inserted into the uterine cavity through the cervix to visualize the inner lining of the uterus. Hysteroscopy done for the purpose of investigation is called Diagnostic Hysteroscopy whereas that which is done for the purpose of surgery is called Operative Hysteroscopy. Hysteroscopy is usually performed just after menstruation. Just like any surgical procedure several complications can occur during and/or after the surgery.
