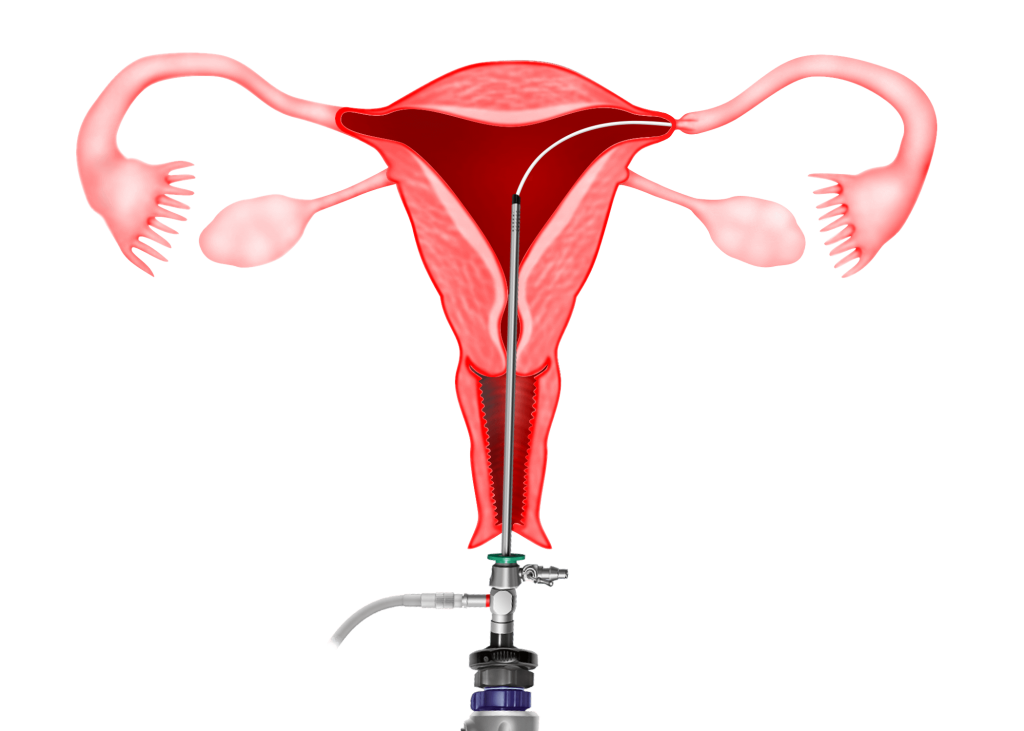
Hysteroscopy is a useful tool in the evaluation of the endometrial cavity in an infertile patient. Hysteroscopy may be performed as a routine for all infertility patients or when an abnormality is found during an ultrasound examination, hysterosalpingography (HSG) or saline infusion sonohysterogram,
The most common surgical procedures that are performed in infertile patients are:
1) Polypectomy
2) Myomectomy
3) Lysis of Adhesions
4) Septoplasty
5) Tubal disease
1) Polypectomy
The removal of an endometrial polyp (see Figures 6.1 and 6.2) is called polypectomy. Small polyps can be removed during an Office Hysteroscopy procedure without anaesthesia whereas larger polyps are removed during an Operative Hysteroscopy procedure under anaesthesia. (see Chapter 36 and 38). The base of the polyp can either be cut using a pair of scissors, diathermy needle or resectoscope. Pregnancy rates are generally believed to improve after the removal of these polyps. (see Chapter 6)
2) Myomectomy
This is discussed in chapter 41
3) Lysis of adhesions
Intrauterine adhesions may be a cause of infertility. Intrauterine adhesions (IUA) are also known as Asherman’s syndrome. Intrauterine adhesions occur:
1) after dilatation and curettage for elective pregnancy termination, missed or incomplete abortions
2) after dilatation curettage is performed to remove a retained placenta, postpartum
3) when dilation and curettage is done in a non pregnant uterus
4) after hysteroscopic, open or laparoscopic myomectomy for submucosal fibroids
5) when there is endometrial infection due to tuberculosis or septic abortion
Diagnosis
Clinical :
Patients with intrauterine adhesions may present with decreased menstrual flow.
Transvaginal ultrasound :
Ultrasound may show a thin endometrium or loculations (cavities) of blood in the endometrial cavity (hematometra)
Hysterosalpingography (HSG) :
HSG may show a small endometrial cavity with filling defects, which are irregular and splotchy.
Hysteroscopy :
A diagnostic hysteroscopy will be able to confirm the diagnosis of Intrauterine Adhesion
Classification
Intrauterine adhesions can be classified into endometrial, myometrial and connective –fiber synechae.
Treatment
Operative Hysteroscopy is the treatment of choice for Intrauterine Adhesions. Mild adhesions can even be lysed during a Office Hysteroscopy procedure. Severe adhesions can be the most difficult and dangerous hysteroscopic procedure because of the loss of anatomical landmarks, resulting in a high risk of uterine perforation (see chapter 36). It is usually best done with the guide of the laparoscope or transabdominal ultrasound to help maintain orientation and limit perforation. Treatment can be done using a pair of scissor, mono or bipolar electrodes or a resectoscope. After recreation of the endometrial cavity, an intrauterine contraceptive device (IUCD) or a balloon catheter can be placed in the endometrial cavity to prevent a recurrence of adhesions. Patients may be given oestrogen therapy for 2-3 months to assist in the regeneration of the endometrial cavity. After the treatment, the IUCD or Folley’s urinary catheter is removed and a repeat hysteroscopy is done to ensure that there are no more adhesions.
Case 40.2 Hysteroscopic lysis of intrauterine adhesions leading to spontaneous pregnancy
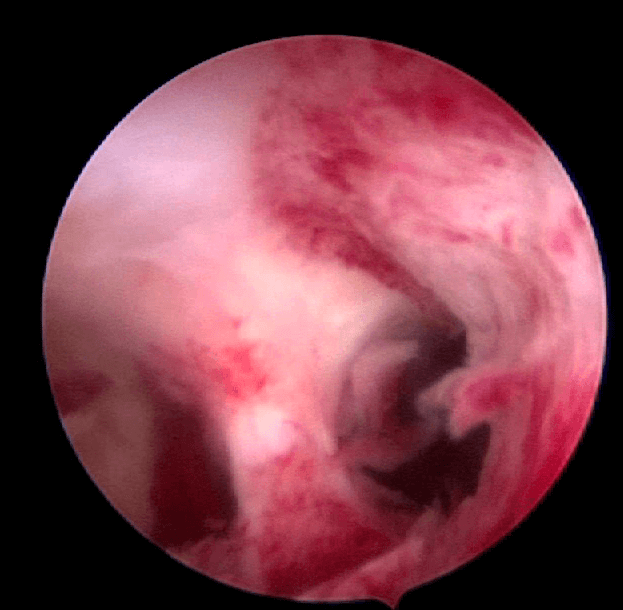
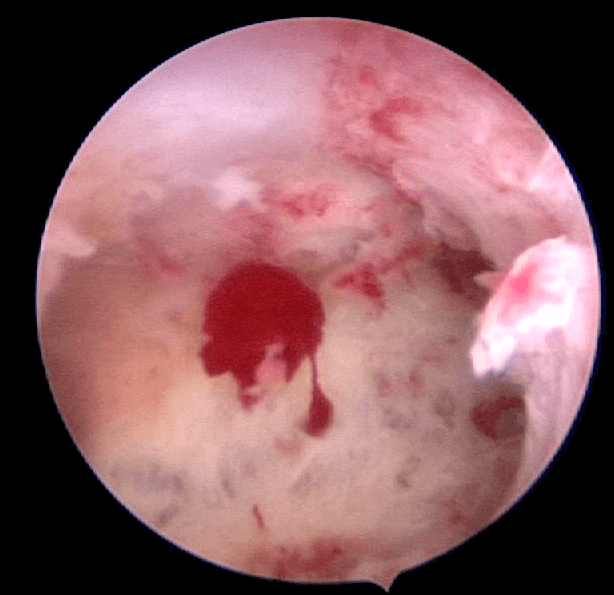
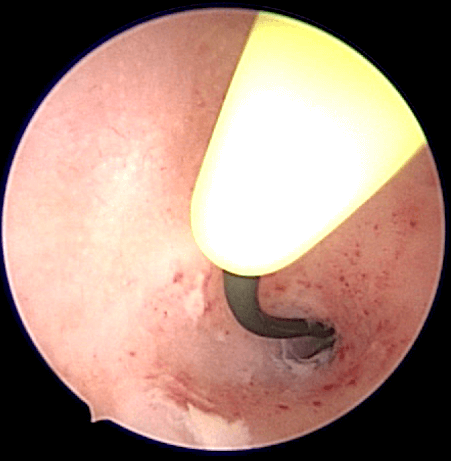
MY a 35 year old lady with regular menses since menarche, miscarried her first pregnancy in June 2010 and underwent a curettage. She did not have any menses after the curettage. She saw a doctor who gave her hormones to induce her menses but she did not get any withdrawal bleeding. She consulted me in October 2010. Examination and ultrasound did not reveal any abnormality. She underwent a hysteroscopy. There was a thick intrauterine adhesions at the fundus of the uterus (Figure 40.2). Adhesiolysis was performed. An intrauterine contraceptive device (IUCD) was placed in the uterine cavity. She was given cyclical hormone replacement therapy for 3 months. She had regular normal menses while on the cyclical hormones. After 3 months of regular menses, the IUD was removed and she was encouraged to conceive. She continued to have regular menses. A few months later she conceived spontaneously and delivered a healthy baby boy.
Discussion
Adhesions in the uterine cavity after curettage for miscarriage is not uncommon and it is called Asherman’s syndrome. It usually presents with the absence of menses after the procedure. The IUCD is placed in the uterine cavity so that the adhesions do not recur. Cyclical hormone replacement therapy medication is given to develop the endometrium so that the patient gets normal regular menses.
4) Septoplasty
Hysteroscopic resection has replaced the older metroplasty done by either laparotomy or laparoscopy. It may be performed under laparoscopic guidance or with transabdominal ultrasound guidance. The septum can be incised using a pair of scissors, diathermy needle, wire loop electrode or laser. The septum is incised from the apex while simultaneously working from side to side continuing cranially until the cavity is flushed across the fundus. If the septum extends to the cervix, this can also be cut although there is a small worry of cervical incompetence.
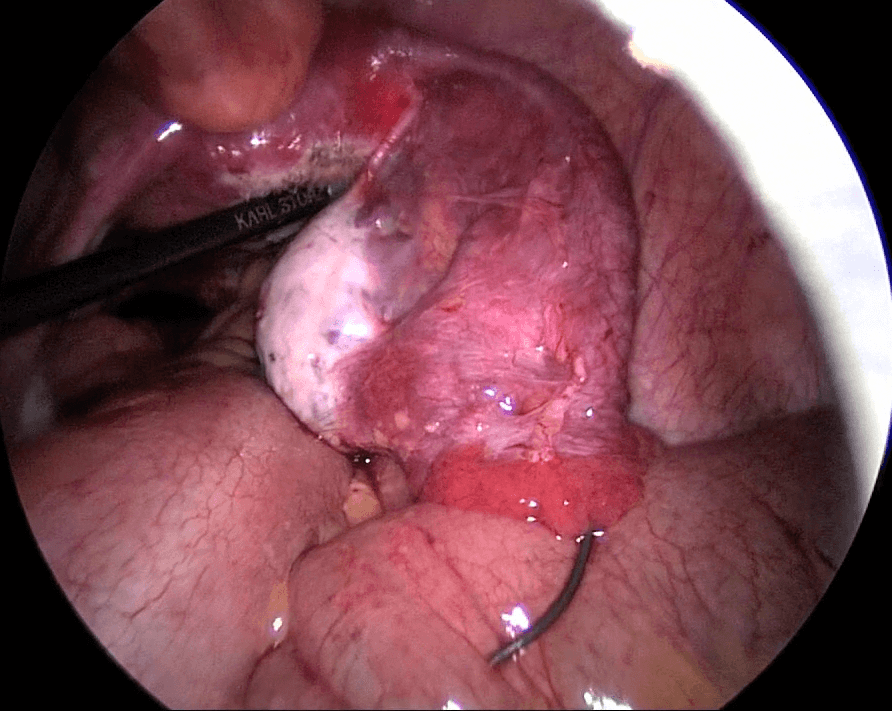
Case 40.1 Hysteroscopic resection of uterine septum which resulted in a spontaneous pregnancy in a woman with 2 previous miscarriages
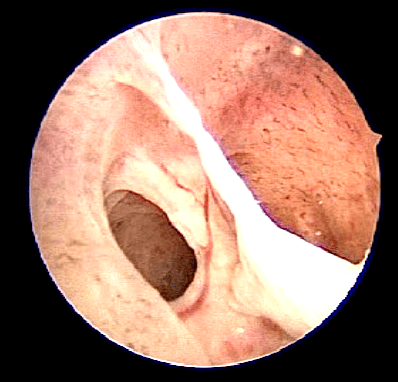
Madam LHS, a 30 year old lady who had 2 previous miscarriages at about 12 weeks of pregnancy consulted me in January 2014. Ultrasound showed a septate uterus (see Figure 40.3). She un- derwent a laparoscopy and hysteroscopy. Incision of the septum was performed hysteroscopically (see Figure 40.4). Both the fallopian tubes were patent. Postoperatively she was well. She conceived spontaneously and delivered a healthy baby girl.
Discussion
Incision of a uterine septum is controversial. Some women with uterine septum can conceive and deliver a full term baby while others may experience miscarriages. Incision of the septum is advisable for women with large uterine septums whereas surgery is only contemplated for women with small septums if they have suffered previous miscarriages.

5) Tubal Block
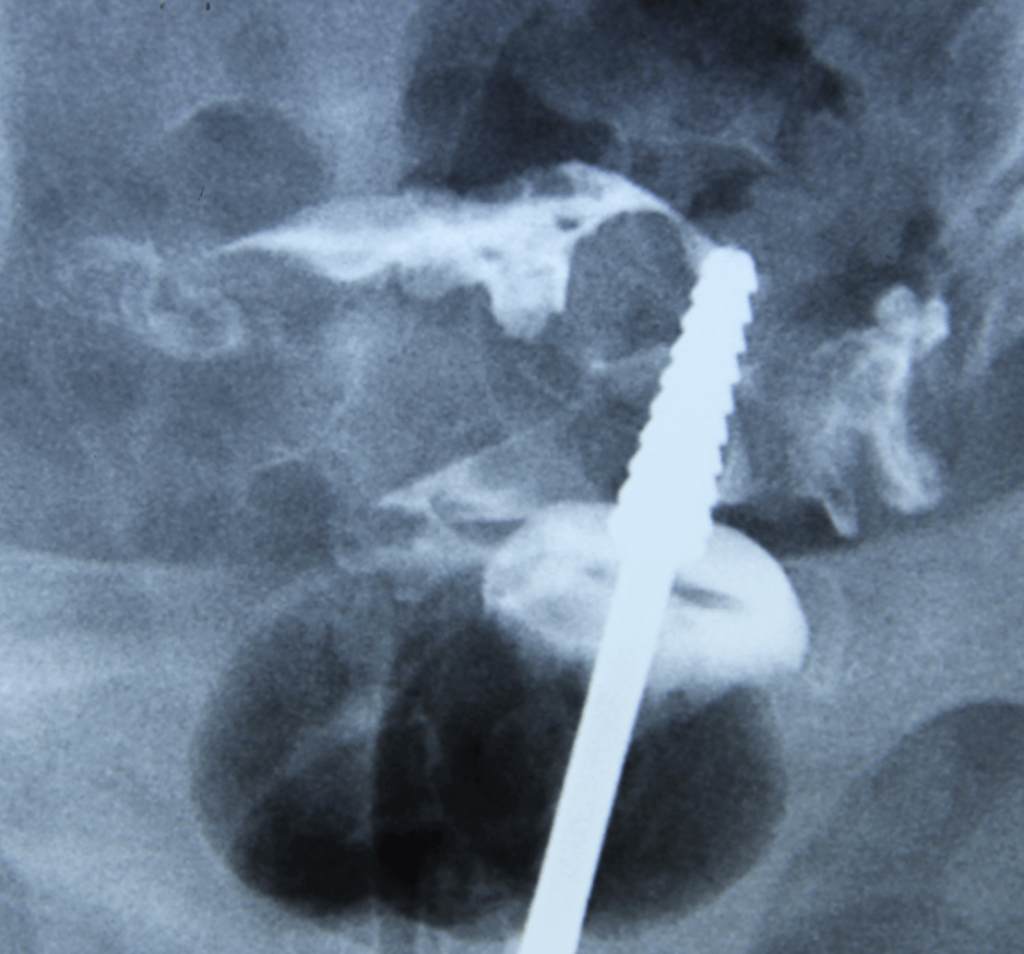
Proximal Tubal Occlusion (PTO) is a condition whereby the tubes appear blocked at the beginning of the fallopian tube on hysterosalpingography (HSG) (Figure 8.2). Bilateral PTO may be due to a congenital abnormality. However unilateral PTO may be due to transient tubal spasm or plugging by mucus, debris or air bubbles. Hysteroscopic tubal cannulation is successful in relieving PTO. During this procedure, a fine catheter is inserted via a hysteroscope to the tubal ostium and dye is injected to open up the tube. If this fails another smaller catheter called a guide wire is passed through the first catheter and advanced into the fallopian tube to open it up. This is usually done while simultaneously performing laparoscopy

Summary
Hysteroscopy is a very useful tool in the evaluation of the endometrial cavity in an infertile pa-
tient. Hysteroscopy aids in the diagnosis and treatment of endometrial pathology or diseases
